Cervical cancer screening typically ends after 65 years of age but many women reach menopause before they age out of the screening process. This will inevitably lead some women to need colposcopy post menopause, especially if they did not receive regular screenings in their younger years and any cervical abnormalities progressed. We spoke to pioneer nurse colposcopist, Dr. Mary Rubin, NP to better understand the challenge of postmenopausal colposcopy and to see how those challenges can be overcome.
The challenges of colposcopy post-menopause
Several factors make colposcopy in post-menopausal women challenging. Vaginal atrophy frequently accompanies menopause, which makes attaining a clear image of the cervix difficult. On the other side of the spectrum, some women find that their vagina shrinks in menopause, making speculum insertion a struggle.
A vaginal retractor can always be used in the case of vaginal atrophy. However, due to the typical lack of lubrication (see below) some women might find the added instrument a painful intrusion. I have found that cutting the end off a condom and placing the sheath over the speculum provides a good ‘make-shift’ solution and then. Once inserted and opened, the condom holds back the lax walls of the vagina without adding additional discomfort to the patient.
Lack of lubrication
For most postmenopausal women, the insertion of the speculum causes discomfort. As the natural level of vaginal lubrication reduces due to the changes in hormone levels post-menopause, it can make the insertion of the speculum less ‘smooth’ for women.
Any form of lubrication, natural or artificial, can interfere with the ability to perform a satisfactory colposcopy. However, as the comfort of the patient is important, I find that applying a water-based lubricant to the lower blade of the speculum improves the experience for the patient while not significantly interfering with the colposcopy procedure.
Changes to the cervix structure

Narrow cervical os seen later in life after the normal maturation process or treatment
of the transformation
Menopausal changes to the cervix pose a particular challenge to the colposcopist. As menopause progresses, the cervical os contracts making it smaller and tighter.
This means that when you examine the cervix using your colposcope, you typically cannot view the endocervix and the squamocolumnar junction. Here, the surface tissue has moved up and into the endocervical canal. This makes the colposcopy procedure more of a ‘fishing expedition’ with endocervical sampling.
Many cases require performing endocervical sampling. The uncertainty caused by difficult imaging means that a more aggressive approach is needed. An abnormality frequently makes it hard to identify the exact location.
Most likely this will necessitate an excisional procedure, not only to remove abnormal tissue but also to make a concrete diagnosis.
Glandular abnormalities
Frequently, in post-menopausal women, abnormal cells result from a glandular abnormality as opposed to an abnormality in the squamous cells. This creates a greater urgency to progress to treatment or, at the very least, for a more frequent visit schedule of further monitoring and evaluation. Due to the overall changes in the cervix structure, gland tissue will have likely moved up into the canal, adding to the need for more aggressive management.
In the case of a Pap test showing a glandular abnormality, in this post-menopause population, you should move directly to colposcopy and not repeat the Pap test as you might in the general population.
Treatment will differ depending on how deeply into the glands the pathology has progressed. In this case, I would not perform cryo- or ablative therapy.
I would move directly to a cone biopsy or LEEP to make a diagnosis and then assess whether all the necessary tissue has been removed in the specimen.
Should high-grade pre-cancer or cancer of the glandular issue be found, it is recommended that the patient have a hysterectomy. This situation is a ‘ticking time-bomb’ and should not be allowed to continue.
Thinner cervical tissue
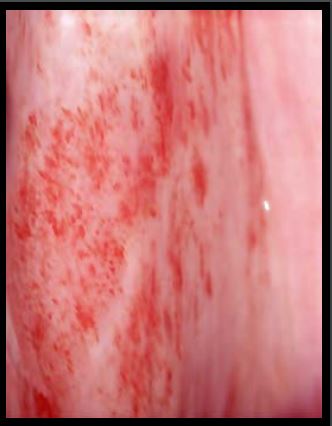
Petechiae seen with inserting speculum over thinning epithelium.
Besides making the os harder to see, some of the changes that the cervix undergoes in menopause can pose a considerable challenge for the less experienced colposcopist. Reduced levels of estrogen causes the surface tissue on the cervix to thin with fewer layers covering the deeper tissue.
This means that the vascular network becomes visible during colposcopy.
The vascular pattern includes many vessels that can mimic the atypical vessels of cancer. You are likely to see vessels that do not branch in the same formation as you would expect to find in a younger patient. This means that often a post-menopausal colposcopy patient will have more biopsies than her pre-menopausal counterpart.
Examining a post-menopausal woman without resorting to taking unnecessary biopsies requires a higher level of colposcopy experience.
When examining a post-menopausal cervix with thinner cervical tissue, it is advisable to be guided by the aceto-whitening changes. However, sometimes the thinner tissue causes the cervix to appear ‘shiny’, which again is likely to lead to numerous biopsies being taken.
Challenges for post-menopause colposocpy patients
For the patients themselves, post-menopausal colposcopy can be very difficult. Due to the issues mentioned above, the procedure feels physically uncomfortable, with patients finding it even less bearable than younger women.
It is quite possible that they will not be able to tolerate the experience for very long. I have known cases where the colposcopy needed to be performed under anesthesia.
I would always advise using the smallest speculum possible. I prefer a small metal speculum for this population as I find that a metal speculum can be inserted more smoothly and with greater control. It is important to avoid causing trauma to the tissue as it can impede your ability to see clearly.
Expert consultation
If you have less experience in colposcopy, then I would advise focusing on younger women of reproductive age until you have better control of the instruments needed. If you do treat a woman of post-menopausal age, it is advisable to consult with an expert colleague.
While you could refer such patients to a colleague for them to perform the colposcopy, it is also possible to use remote digital consultation to allow a colleague to supervise the procedure via a digital connection. Specialist equipment is required for a medically suitable, HIPAA compliant connection. Such a system is well worth the investment as it enables any clinician to provide advanced level care.
Learn how the EVA System enables you to consult with remote colleagues >>