Colposcopy
Explained
What is it,
what to expect, and
how to prepare
Why would I need a colposcopy?
If you have an abnormal Pap test result or your HPV test came back positive, then your doctor or nurse may send you to have a colposcopy procedure. You might also have a colposcopy performed if you have experienced painful sex, unexplained vaginal bleeding or bleeding after sex to look for possible explanations of these symptoms.

What exactly is a colposcopy?
Colposcopy is the magnified visual inspection of the cervix to check for any abnormalities. In other words, your doctor or nurse is going to look at your cervix to check for any signs of problematic cells growing.
Does this mean that I have cervical cancer?
No! A colposcopy is a test to evaluate for any changes on your cervix that could become cancer in the future. It does not mean that you have cancer now. Cervical cancer can take 10-15 years to develop which is why regular screening can prevent abnormal cells from ever developing into cancer. If your doctor or nurse said that you need one, then having a colposcopy is the best way to make sure you don’t develop cervical cancer.


What would happen if I didn’t go to the colposcopy procedure?
It all depends on your cervix. If there are abnormal cells present, then they could develop into cervical cancer. If there are no abnormal cells growing, then nothing will happen. The only way to know what is happening on your cervix is to go for the colposcopy and find out.
What to do before a colposcopy:
- Avoid using vaginal medication, personal lubricants or douches for 48 hours before the colposcopy.
- Refrain from vaginal sex for 48 hours before your appointment.
- Schedule your appointment on a day when you do not have your period.
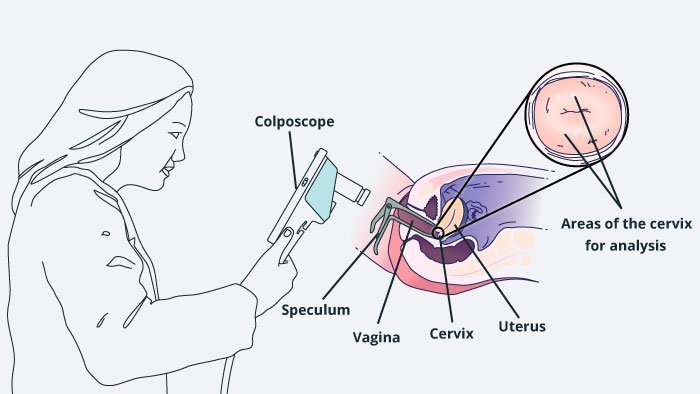
What happens during a colposcopy?
You will either change into a hospital gown or remove your clothes from the waist down. You will lie on your back on an exam table and place your feet in the foot holders (stirrups) on either side of the bed with your knees in the air.
Next, they will apply a vinegar solution to your cervix with a swab (like a big Q-tip.) This vinegar solution whitens any problematic areas on your cervix giving a clear view of areas that need more attention.
The clinician will insert a lubricated speculum into your vagina. This holds back the vaginal walls to enable the clinician to see your cervix clearly. You will feel some pressure as the speculum is inserted.
Your clinician will then use a colposcope to look at your cervix. A colposcope shines a bright light on your cervix and magnifies the image so the clinician can see clearly if any areas look suspicious. Depending on the type of colposcope used by your clinician, they may be able to show you a picture of your cervix or even the live feed of what they’re seeing.
If any areas look potentially problematic, the clinician may perform a biopsy. This involves taking a tiny sample of the tissue from your cervix to send to a lab for analysis. It will feel like a sharp pinch. You might feel cramping, similar to menstrual cramping. Your clinician might need to take more than one biopsy depending on what they see.
What to do after a colposcopy:
Your vagina might feel a little sore for a few days after colposcopy. You may experience some cramping similar to menstrual cramping for a day or two afterward. If you had a biopsy then you will probably experience some bleeding immediately afterward, with slight spotting or dark-colored discharge for a few days afterward. You can use a pad or panty-liner. Avoid using tampons.
- You can shower as soon as you want (wait 24 hours before taking a bath).
- Wait 24-48 hours to have vaginal sex or until bleeding stops if you had a biopsy.
- Contact your doctor if you experience heavy bleeding, have smelly vaginal discharge or fever.
CERVICAL CANCER SCREENING RECOMMENDED SCHEDULE IN THE US:
Women aged 21-29
it’s recommended to have a Pap test every 3 years. HPV testing is not recommended.
Women aged 30-65
It’s recommended to have a Pap test and an HPV test (co-testing) every 5 years. It is also acceptable to have a Pap test alone every 3 years or HPV test alone every 5 years after the age of 30.
See here for more information:
https://www.acog.org/Patients/FAQs/Cervical-Cancer-Screening-Infographic
This table is a guide from the American College of Obstetricians and Gynecologists to general screening frequency in the US. Some women might have other needs, and some countries follow different guidelines. Consult your healthcare provider to confirm your individual screening schedule.
What is next after the colposcopy procedure?
If your clinician did not find any abnormalities, you can follow up for a routine cervical cancer screening. Your clinician will recommend the appropriate time to come back according to the accepted screening guidelines.
If any biopsies were taken, you will need to wait for the results before your clinician will recommend the next step in your treatment plan. The biopsy will tell if the sample was normal or abnormal. If abnormal, the biopsy will help determine the level of severity which will guide the next steps in management.
What if I do have an abnormality?
If abnormalities are found, your clinician may recommend a procedure to remove the problematic cells to prevent them from growing or spreading. In most cases, the procedure will just take one appointment with either your clinician or another specialist to remove the cells.
In the unlikely case that you need more extensive treatment, your clinician will walk you through the next steps.
HOW LIKELY AM I TO HAVE CERVICAL CANCER?
About 1 in 20 women will have a smear test result which is abnormal, but only about 1 in 2000 will have cervical cancer with any grade of abnormal smear.
So if you had an abnormal Pap smear test, you still only have about a 1% chance of having actual cervical cancer.
However, over 15,000 women in the USA develop cervical cancer, mainly because they skipped primary or secondary screening, so make sure you attend your primary screening and colposcopy appointments.
More Information:
There are many reliable sources of information online for you to learn even more about colposcopy. Feeling empowered with a full understanding of the procedure will help reduce stress and improve your experience. Here are a few places to start:
AAFP: Colposcopy information page – https://familydoctor.org/colposcopy/
CDC: What you need to know about cervical cancer – https://www.cdc.gov/cancer/cervical/index.htm
NHS: What happens in colposcopy – https://www.nhs.uk/conditions/colposcopy/what-happens/
ASCCP: Official US colposcopy guidelines – http://www.asccp.org/asccp-guidelines
BSCCP: British Colposcopy Society FAQs – https://www.bsccp.org.uk/women/frequently-asked-questions/
NOTE: Many of these materials are based on the American Association of Colposcopy and Cervical Pathology (ASCCP) materials and guidelines. All information, content, and material of this website for informational purposes only and are not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.
Support groups:
Help is out there from other women who have been through a colposcopy procedure. Hearing from others who have had questions and concerns just like yours and knowing you are not alone in this process can make the procedure a little less scary. Many organizations and online support groups share personal stories, medical information, and advice, as well as resources for financial assistance with treatment.
CANCER CARE
Nonprofit offering counseling, support groups, cancer education, and financial assistance
https://www.cancercare.org/diagnosis/cervical_cancer
CERVIVOR
Non-profit raising awareness about cervical cancer, education for advocates and allies, giving support to patients.
CANADIAN CANCER SOCIETY
Offers support for cancer patients including medical guidance, financial assistance, online support groups.
http://www.cancer.ca/en/cancer-information/cancer-type/cervical/cervical-cancer/
CANADIAN WOMEN’S HEALTH NETWORK
An advocacy group raising awareness and giving information about women’s health issues. Website in English and in French.
http://cwhn.ca/en/yourhealth/faqs/HPVandCervicalCancer

CANCER ASSOCIATION OF SOUTH AFRICA
Funds cancer research, providing education about cancer screening and risk reduction, supporting cancer patients.
https://www.cansa.org.za/womens-health/
Jo’s CERVICAL CANCER TRUST
Nonprofit offering support, information, and educational materials about cervical cancer
THE EVE APPEAL
A Nonprofit raising awareness and giving support for gynecological cancers, including cervical cancer
THE IRISH CANCER SOCIETY
Offers support and information for cancer patients, including confidential telephone support and in-person.
https://www.cancer.ie/cancer-information/cervical-cancer#sthash.gkEWqVTG.dpbs
THE MARIE KEATING FOUNDATION
Provides cancer information and support for patients and families
https://www.mariekeating.ie/cancer-information/cervical-cancer/

AUSTRALIAN CERVICAL CANCER FOUNDATION
Offering support for cervical cancer patients and families, raising awareness through community and school programs.
CANCER COUNCIL PINK RIBBON
Raises awareness about breast and gynecological cancers.
https://www.pinkribbon.com.au/nt/women-and-cancer/cervical-cancer
NEW ZEALAND CANCER SOCIETY
Support for cancer patients including information nurses, transport to treatments; raising awareness about cancer-related issues; research funding.
https://cancernz.org.nz/cancer-information/cancer-types/cervical-cancer/